Archimedes is not a household name any longer, though had Popular Science been around during his life in 230 BC, he might have been a frequent face for the cover story. Still, we reap even today many of the benefits of his observations, calculations, and inventions. His claim, “Give me a lever long enough and a fulcrum on which to place it and I shall move the world,” underscored the multiplier effect of that simple machine, the lever. Today, facing enormous challenges in global healthcare, it is tempting to ask whether there are not other basic innovations that have the power to move the mountainous problems of our day if we only have those two key elements—a lever and a fulcrum. May I presume to posit that digital pathology (the application of digital imaging technologies to pathology and diagnosis of human disease, DP) is just such a long enough lever, and augmented/artificial intelligence (AI) may be the fulcrum that allows it to multiply its power over some of our key global healthcare mountains.
Let’s take four key challenges in global health to illustrate how this might prove to be true. Looking ahead, using reasonable projections of disease incidence, aging populations (of both patients and workers), and economic projections, there are four trends that should give us serious pause.
- GLOBAL DISPARITIES
The first is the vast global health disparities that exist now and face the potential to expand as the disease burden of non-communicable diseases grows in the lower-resource countries of the world. For example, cancer annual incidences are expected to increase by 75% over the next 25 years, while population growth will only be 21%, and a disproportionate number of these added cases will occur in developing countries. As seen in Figure 1, 20% more cancer cases will occur in Africa compared to North America, and similar disparities also exist for Latin America and Asia. In addition to the cancer burden inequities, many of these same areas still carry an inordinate number of infectious diseases, such as malaria, filariasis, and tuberculosis, and they are now seeing increased cardiovascular disease, diabetes, and obesity as they develop.
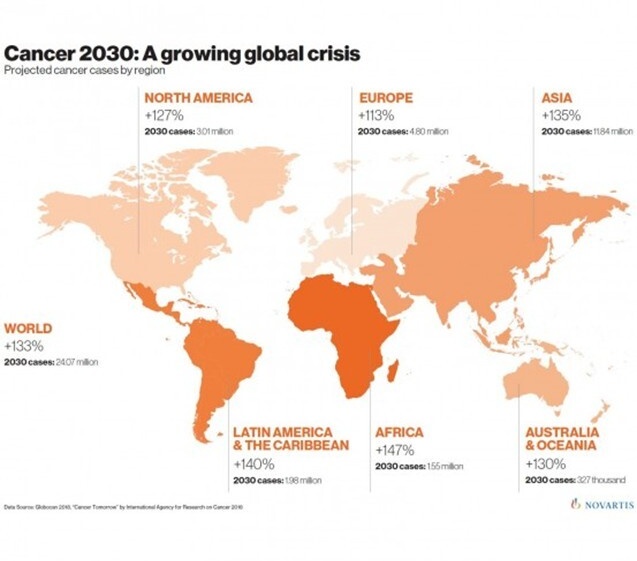
Figure 1 Cancer Incidence Projections for 2030. Data from IARC sources, graphic courtesy of Novartis.
- WORKFORCE (IN)ADEQUACIES
A second mountainous problem is the workforce shortage in medicine generally and in pathology and lab medicine in particular. In the US, this is due to a fairly tightly controlled input, coupled with the demographic wave of an aged workforce moving into retirement. In many other areas of the world, limited or absent training programs, coupled with “brain drain” emigration and other social, political, and economic factors, have made this a very serious problem.
- RISING HEALTHCARE COSTS
Rising costs in the healthcare sector also loom as a huge problem. With such costs consuming nearly 20% of the US Gross Domestic Product annually, and continuing to increase, economic catastrophe seems a strong possibility. Rationing of care in economically less developed countries highlights social divisions, fostering political instability as well.
- DATA SILOS
A fourth issue is the serious data “silo-ing” that precludes optimal care, tool development, and proper planning and resource allocation. Despite efforts to break down some of these silos through legislation or consolidation, or to at least create pipelines between them, patient privacy, proprietary concerns, and even issues like national security can persist in keeping these valuable resources locked away from the public good.
For some of these big rocks, the manner in which DP and AI interplay to mitigate their impacts may be obvious, but for others, less so. Let me explain how they may shift these problems into the “solved” column on the scoresheet. DP is a great equalizer and has the potential to do to diagnostic pathology what the internet did to global communications. A few decades ago, costs for international and even domestic calling were prohibitive, whereas now it is essentially a free service. Today I consulted on a case seen yesterday in Hanoi and another from Malawi, and was able instantaneously to share the issues and even the slides from those with colleagues in London, Pittsburgh and Florida, without charge or much in the way of time delay. Access and efficiency are key impacts of DP. But even further, this week my colleagues in the OPEN Pathology Education Network (OPEN) helped train budding pathologists in Mongolia, Cambodia, Africa and the US using curated DP educational materials. AI assistance captured portions of those sessions to help bridge communication and time zone chasms. DP, along with AI, is helping us (in OPEN and other settings) to address the workforce gaps that a traditional pathology education model cannot solve in any reasonable time frame.
Similarly, many of the AI diagnostic adjunctive tools being developed offer the hope of significant increases in pathologist productive capacity. For example, a recent study of breast biopsies studied in an AI-adjunctive manner showed a 23% reduction in review time and a 33% reduction in immunochemistry orders. Coupled with the improvements offered by a digital workflow, we may see gains of up to 50% in some settings, particularly where the implementation is optimized for workflow efficiency. In another context, AI tools have been developed to screen stool samples for ova and parasites, thus compensating for waning or weak expertise in parasitology. The tools are in use in at least one large reference laboratory in the US, but would appear to offer promise to areas with high disease burden as well.
DP and AI also show glimmers of hope in reducing costly inputs needed to arrive at a diagnosis. Should technologies like Fluorescent-imitating brightfield illumination (FIBI) or other tissue direct to digital (H&E-like) imaging, or virtual staining algorithms prove robust, the cost paradigm for pathology would shift dramatically. These technologies allow direct imaging of fresh or fixed, and even paraffin-embedded tissues, and thus potentially preclude the need for overnight processing and other functions and equipment of a histology laboratory, and can provide much more rapid access to diagnostic digital images amenable to AI analysis. FIBI prototypes are in clinical trials in several areas, already funded by grants. Furthermore, the extraction of molecular genetic information from digital pathology images also portends a disruption in the cost structures of pathologic diagnosis-dependent care. To date, numerous studies of a host of genetic biomarkers (>20) have shown success in identifying biomarker status from WSI, all with areas under the receiver-operator curves of >65%. While those results may not presently completely displace conventional methods, the potential to begin to use such testing with high predictive values to include or exclude patients from study or access to drugs much more rapidly and less expensively appears promising.
Clayton Christensen’s theories of disruptive innovation grew out of observations in the technology sector but he courageously encouraged their application in education, healthcare and economic development of entire nations. Often, he observed that disrupting innovations entered with a “no-frills” product that was better than nothing, in a new market where no prior solution or service had been available. Well, might we ask whether a DP and AI solution largely independent of pathologists might be considered for underserved populations in Africa, Lao, or other areas? Innovations such as 3D-printed microscopes and scanners, coupled with low-cost solutions like FIBI, could be cost-permissive DP implementations in limited-resource settings. The moral and ethical constraints around such an implementation are far from trivial, but the question warrants consideration and meaningful discussion, given the equity and workforce challenges alluded to above.
Finally, the pressures to access multiple data sources so that these tools can be developed are helping to fuel models such as the federated model for sharing data without risking loss of ownership or beneficial interests.[1] So even here, the drive to develop AI using DP and other data sources may partly at least help to smash this last mountain barrier.
Archimedes was right. Leveraged efforts can change the world. Seeing even the beginning incremental shifts DP and AI are bringing against these four stubborn problems gives me hope we are going to get there.
Lewis Hassell, MD
Professor of Pathology
University of Oklahoma Health Sciences Center

[1] A federated model for data sharing is a decentralized approach where data stays on local devices or within separate organizations, and only aggregated model updates or query results are shared to build a collective outcome, rather than moving raw data to a central location. This model enables collaboration while preserving data privacy and security, making it ideal for sensitive datasets like medical records or financial information
1 comment(s) on "Is Digital Pathology and Augmented/Artificial Intelligence Archimedes’ lever to lift the world?"
11/25/2025 at 10:51 PM
Michael Henderson says:
Dr. Hassell, thank you for this thoughtful reflection. As an early adopter and implementer of both digital pathology and AI, I share your optimism about their potential—but that experience is precisely why I believe disciplined governance must accompany scale.Leverage amplifies everything, including unintended consequences. Access does not automatically confer equity, efficiency does not guarantee preserved expertise, and data sharing demands stewardship, not assumption.
I would also caution against too casually invoking the internet as proof of inevitable societal benefit. The dot-com era brought extraordinary innovation, but also bubbles, monopolization, and persistent inequities. Global reach did not translate into universal equity. That analogy deserves examination, not creed.
If DP and AI are to mature responsibly in medicine, they must be adopted with rigor, accountability, and continual ethical scrutiny—not just enthusiasm. I appreciate this contribution and the important discussion it invites.
Please log in to your DPA profile to submit comments